Living with epilepsy can feel like navigating life with an invisible storm—unpredictable, disruptive, and often misunderstood. However, epilepsy is more than just seizures. It also affects physical health, emotional well-being, and social connections. Nevertheless, with the right support and lifestyle adjustments, individuals can lead fulfilling lives. Despite medical advancements, the stigma surrounding epilepsy continues to create challenges, leaving many isolated. In addition, this article shares practical strategies to manage seizures, improve daily life, and break through the misconceptions, empowering those living with epilepsy to reclaim their well-being and thrive.
Tips for Living with Epilepsy and Improving Your Life
Living with epilepsy involves managing not only seizures but also the broader impact on daily life. Lifestyle changes, practical tools, and robust support networks can significantly improve the quality of life for those affected by the condition.
Stress Management Techniques
Stress is a common cause for seizures, making its management vital. Practices like mindfulness, yoga, and relaxation techniques can help regulate the nervous system and reduce the likelihood of stress-induced episodes:
- Mindfulness: Guided meditations and deep breathing exercises help patients focus on the present moment, alleviating anxiety associated with the unpredictability of seizures.
- Yoga: Gentle practices like restorative yoga can enhance relaxation while promoting physical and emotional well-being.
- Relaxation Therapy: Techniques such as progressive muscle relaxation offer practical ways to ease tension in daily life.
The Role of Sleep in Controlling Seizures
Poor sleep or irregular routines can exacerbate seizure risk. Key strategies include:
- Maintaining Consistent Sleep Patterns: Going to bed and waking up at the same time each day to regulate brain activity.
- Creating a Sleep-Conducive Environment: Reducing screen time, keeping the bedroom dark, and using white noise if needed.
- Avoiding Stimulants: Limiting caffeine and alcohol intake before bedtime, as these can disrupt sleep quality.
Dispelling Myths and Breaking Stigma Surrounding Epilepsy
Myth: People with epilepsy are a threat to society
Surveys and interviews reveal that individuals with epilepsy are often wrongly perceived as dangerous or unstable. This misconception stems from a lack of understanding about the condition, which is neurological and does not pose any inherent risk to others. Such views lead to discrimination in schools, workplaces, and communities.
Myth: Epilepsy is caused by possession or supernatural forces
Despite advances in medical science, some communities still associate epilepsy with possession by spirits or demons. This outdated belief not only stigmatizes individuals but also discourages families from seeking medical treatment, opting instead for spiritual remedies that can delay proper care.
Myth: Epilepsy is contagious
A persistent myth in some regions is that epilepsy can spread through physical contact or proximity. This baseless belief isolates individuals, depriving them of social interactions and support systems. Scientific evidence confirms that epilepsy is not contagious.
Myth: People with epilepsy cannot lead normal lives
While epilepsy can pose challenges, with proper treatment and support, most individuals can live fulfilling lives. Misconceptions that they are incapable of achieving academic or career success create unnecessary barriers. Many individuals with epilepsy have excelled in various fields.
Myth: Epilepsy is untreatable
Advances in medicine, including medications, surgical options, and neurostimulation therapies, have made epilepsy manageable for most patients. However, the myth that it is untreatable persists, leading to despair and misinformation.
Myth: People with epilepsy are mentally ill
While epilepsy may sometimes co-occur with mental health conditions, the two are distinct. Labeling individuals with epilepsy as mentally ill perpetuates stigma and ignores the neurological basis of the condition.
Myth: Epilepsy doesn’t require medicine
Some people believe that epilepsy can be managed without medical treatment, suggesting traditional remedies like making a person smell a shoe. This misconception endangers individuals by delaying access to effective treatment.
Myth: Only convulsions are considered seizures
There is a lack of understanding that epilepsy can present in different forms, such as absence seizures or myoclonic jerks, leading to the invalidation of other seizure types.
Myth: Epilepsy affects marital prospects
A prevailing notion is that epilepsy makes individuals, particularly women, undesirable as marriage partners. This belief perpetuates stigma and creates unnecessary emotional and societal barriers.
Myth: Harmful seizure “management” practices
Outdated practices, such as forcing a spoon into a person’s mouth during a seizure, continue to be propagated, leading to harm rather than helping the individual.
Myth: Social pressure to conceal diagnosis
Many people with epilepsy are encouraged to hide their condition to avoid judgment, leading to isolation and a lack of support.
Raising Awareness: Combating Stigma Through Advocacy and Education
Living with epilepsy often means facing not just seizures but also the stigma that limits opportunities in education, employment, and personal relationships.
Misinformation, fear, and stereotypes fuel this stigma. Therefore, combating it demands collective action, fostering empathy, and promoting awareness on a global scale.
Effective Strategies to Raise Epilepsy Awareness
- Public Campaigns
Initiatives like Purple Day for Epilepsy serve as powerful tools to raise awareness. For instance, on this global day of advocacy, communities unite to educate people, dispel myths, and show solidarity with individuals living with epilepsy. Additionally, social media drives, public seminars, and community events create platforms for open dialogue and education. - Education in Schools and Workplaces
Integrating epilepsy education into schools and workplace training programs builds informed and empathetic environments. By doing so, we teach peers, teachers, and employers about seizure first aid, address misconceptions, and promote inclusivity. Ultimately, this ensures individuals with epilepsy feel supported, not isolated - Personal Advocacy
Stories hold incredible power. In particular, when individuals with epilepsy and their families share personal experiences, they humanize the condition and challenge stereotypes. As a result, these narratives deepen understanding, inspire others to support the cause, and encourage allies in the fight against stigma.
By combining public campaigns, targeted education, and personal advocacy, we can build a world where people see epilepsy not as a limitation, but as one part of a person’s life. These efforts are essential to ensure individuals with epilepsy lead fulfilling lives free from societal prejudice.
Case Study: Living with Juvenile Myoclonic Epilepsy
In the summer of 2019, doctors diagnosed Sarah with Juvenile Myoclonic Epilepsy (JME), a condition characterized by jerking movements in the arms or legs, often occurring upon waking. The diagnosis came shortly before her fifteenth birthday, bringing a sense of relief. Before this, Sarah had experienced myoclonic seizures for years, but the underlying cause remained unclear. These seizures typically occurred in the morning while she performed routine tasks—like holding a glass of milk or her spectacles—which led to involuntary arm jerks that caused her to drop objects. As a result, the diagnosis was a significant turning point for Sarah.
Although initially manageable, Sarah’s condition took a drastic turn in 2019 when she experienced a full-blown seizure with convulsions. This episode followed a night of insufficient sleep, competition-related stress, and several cups of black coffee. Consequently, her family sought medical consultation, which ultimately confirmed the JME diagnosis. While some individuals with JME experience absence seizures (brief episodes of staring), Sarah did not exhibit this symptom. Instead, she dealt with excessive blinking and persistent hand tremors, which further complicated her condition.
Following the diagnosis, doctors began treating Sarah’s condition with Valproic acid (Valporal CR), which successfully stopped the seizures. Over time, they adjusted the medication dose to maintain seizure control. Despite these adjustments, Sarah still occasionally experiences leg jerks during sleep. At one point, her doctor prescribed Levetiracetam for a short period, but after careful evaluation, it was discontinued due to limited effectiveness.
In terms of lifestyle, Sarah faces relatively few restrictions. She drives and cooks but avoids swimming, drinking alcohol, and prolonged screen time. Her doctor encourages her to sleep about eight hours each night and avoid being startled awake. Additionally, during one conversation, her doctor discussed the possibility of adjusting her medication if she decides to marry or have children, but this topic has yet to be revisited.
Despite her medical progress, Sarah continues to face challenges related to stigma. While her family has been supportive—particularly since epilepsy runs in the family—society’s misconceptions about the condition have created significant hurdles. For example, some communities perpetuate myths, such as attributing seizures to possession or claiming they can be “treated” by smelling a shoe or placing a spoon in the mouth. These outdated beliefs have caused isolation and unwarranted shame for Sarah. In some cases, people have even advised her to hide her condition to avoid judgment or difficulty finding a marriage partner.
Nevertheless, through determination, proper treatment, and the unwavering support of her family and medical professionals, Sarah has built a fulfilling life. Her journey underscores the importance of managing epilepsy effectively and challenging harmful stigmas. By raising awareness, we can create a more inclusive and understanding environment for individuals living with epilepsy.
Practical Steps for Supporting Individuals with Epilepsy
Be Respectful of Their Independence
Encourage individuals with epilepsy to manage daily tasks independently. Offer help only when they request assistance to respect their autonomy.
Support Medical Management
Remind them to follow their medication schedules, attend appointments, and maintain a seizure diary. Help them track seizure patterns and manage their condition effectively.
Create a Safe Environment
Remove sharp or dangerous objects from their surroundings to reduce the risk of injury during a seizure.
Offer Emotional Support
Listen actively to their experiences and validate their feelings. Build trust by encouraging open and honest communication.
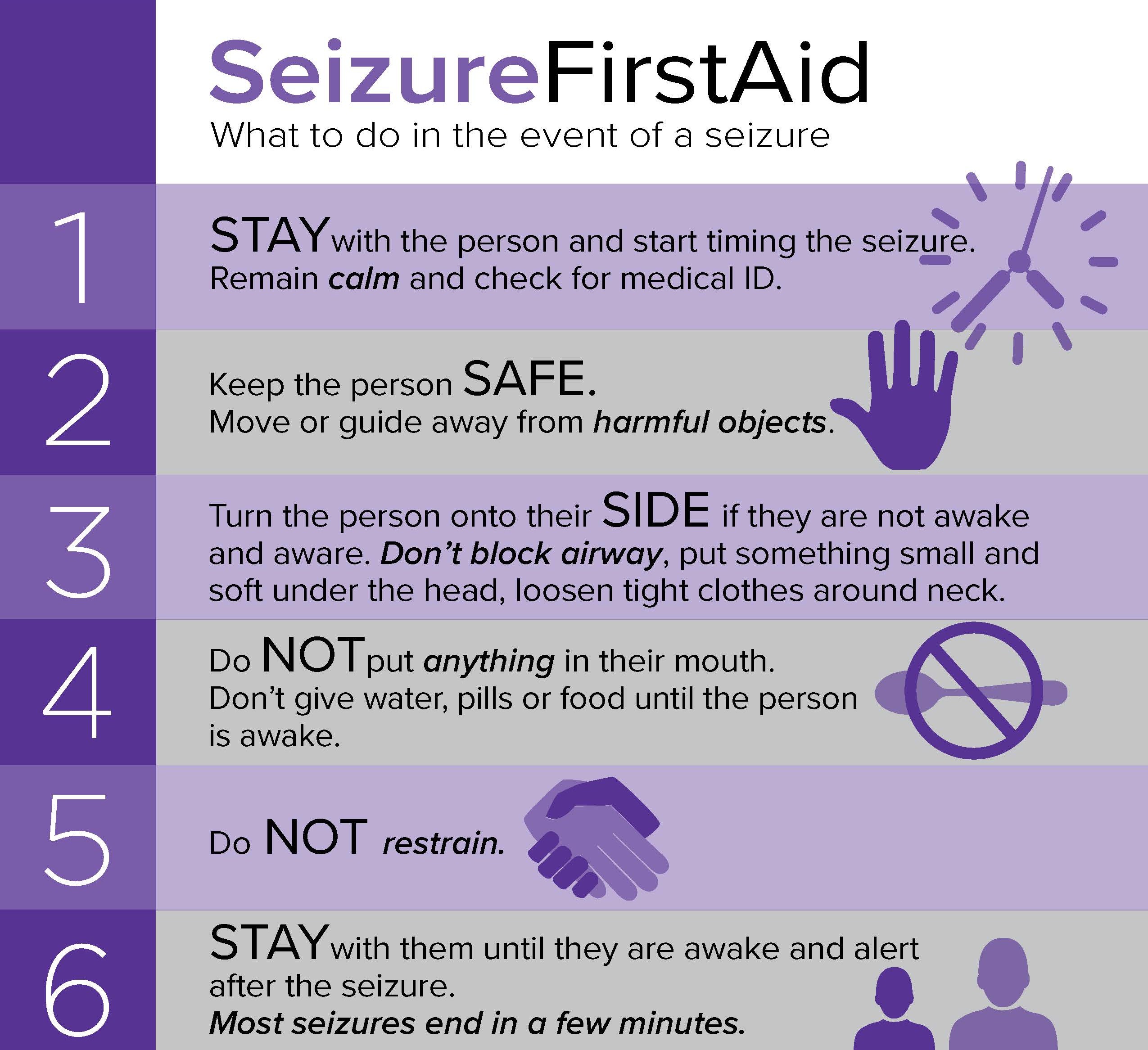
Responding to a Seizure
- Stay calm and clear harmful objects from their immediate area to keep them safe.
- Time the seizure and seek emergency assistance if it lasts more than 5 minutes or happens repeatedly without recovery.
- Avoid putting objects in their mouth unless a healthcare provider instructs otherwise.
Use Appropriate Tools
Administer a prescribed nasal inhaler (e.g., midazolam) to stop a seizure quickly. Follow healthcare instructions for all tools to ensure proper use.
Epilepsy is more than a neurological condition; it impacts every aspect of a person’s life. Integrating medical advancements with emotional support and community advocacy dismantles stigma and empowers individuals living with epilepsy. Together, we create a world where epilepsy no longer limits anyone’s potential.
If you found this article helpful, you might also like to dive deeper into understanding epilepsy with our comprehensive guide: Understanding Epilepsy: The Role of Healthcare and Support
References:
Case Study : Sarah’s Journey with Juvenile Myoclonic Epilepsy
Ayushi Tyagi . (2024). Case study on living with Juvenile Myoclonic Epilepsy. Personal communication.
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1269241/full
https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2021.753753/full
https://www.who.int/news-room/fact-sheets/detail/epilepsy
https://www.epilepsy.com/stories/epilepsy-and-psychological-disorders
https://www.epilepsy.com/tools-resources/forms-resources/first-aid